Headline News
DISTINCT CLINICAL AND RADIOGRAPHIC PHENOTYPES IN PEDIATRIC PATIENTS WITH MOYAMOYA

July 1, 2021
DISTINCT CLINICAL AND RADIOGRAPHIC PHENOTYPES IN PEDIATRIC PATIENTS WITH MOYAMOYA
Kaseka ML, Slim M, Muthusami P, Dirks PB, Westmacott R, Kassner A, Bhathal I, Williams S, Shroff M, Logan W, Moharir M, MacGregor DL, Pulcine E, deVeber GA, Dlamini N.
https://www.pedneur.com/article/S0887-8994(21)00048-5/fulltext
Kaseka et al. carried out an important study to compare the clinical and radiographic differences of children with Moyamoya Disease (MMD) and Moyamoya Syndrome (MMS), to identify prognosticators of recurrent stroke. They further subdivided the MMS patient population into two subgroups MMS-NF1 (Neurofibromatosis type 1) and MMS-SCD (Sickle cell disease) and compared these distinct populations to patients with MMD. A total of 111 children were included. Radiographic characteristics examined included presence of bilateral or unilateral disease, ivy sign, cerebrovascular reactivity (CVR), ischemic event recurrence, radiographic progression, asymptomatic disease, and impact of surgery. Their results are as follows: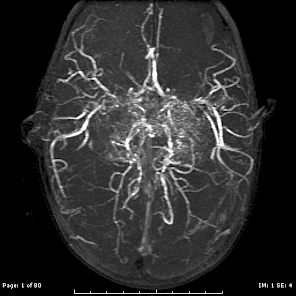
- Patients with MMS-NF1 demonstrated a more benign course of disease evolution with less ischemic event recurrence. This was thought to be related to lower prevalence of bilateral disease compared with patients with MMD and MMS-SCD.
- Patients with MMS-SCD were more likely to have bilateral disease and less likely to demonstrate the ivy sign.
- The ivy sign did not correlate with infarction risk at presentation or with long-term motor and cognitive outcomes.
- Patients of European descent were less likely to have further TIA compared with patients of East Asian descent.
- Frequent TIAs were more common in MMD. Symptomatic stroke presentation was more common in MMD and MMS-SCD.
This study highlights that moyamoya has variable features depending on the related disease, supporting a personalized approach to caring for these children. Specifically, patients with asymptomatic MMS-NF1 and a reassuring CVR warrant a more conservative approach to management.
![]()
Melike Guryildirim, MD
Johns Hopkins Medicine