Headline News
ASNR 2020 PEDIATRIC OUTSTANDING PRESENTATION AWARD

ASNR 2020 PEDIATRIC OUTSTANDING PRESENTATION AWARD
Congratulations to doctors S. Dakil, R. Clarke, J. Tweed, C. Greenwell, and T. Booth from UT Southwestern Medical Center, Dallas, TX for winning the ASNR 2020 Pediatric Outstanding Presentation Award for “ Incidence and Clinical Predictors of Intracranial Hemorrhage in Children with Non-accidental Trauma”.
Here is the list of ASNR 2020 Pediatric Neuroradiology Submissions:
- The Anterior Chamber of the Eye: An Overlooked Entry of the Natural Excretion pathway of Gadolinium Based Contrast Agents?
- In-Utero Tractography of the Cerebellum in the Third Trimester of Pregnancy.
- Incidence and Clinical Predictors of Intracranial Hemorrhage in Children with Non-Accidental Trauma.
- Obstructive Sleep Apnea Impacts Brain Development in Obese Children and Adolescents: an MRI Study.
- Traffic-Related Air Pollution Associated with Altered Neuroimaging Outcomes in a Longitudinally Studied, Pediatric Cohort.
- Characteristics of Pediatric Patients with Traumatic Epidural Hematomas Who Can Be Safely Observed: A Clinical Validation Study.
- Interhemispheric Perfusion Asymmetry from Circle of Willis Arterial Maturity in Normal Population.
- Imaging and Management of Iatrogenic Pseudoaneurysm and Arteriovenous Fistula in a Neonate Post Lumbar Puncture.
Finally, many thanks to the hard-working ASPNR Awards Committee chaired by Mark Mamlouk MD and the committee members Bill O’Brien, Judy Gadde, Julie Guerin, Steve Kralik, and Asha Sarma for diligently reviewing and scoring all submissions!
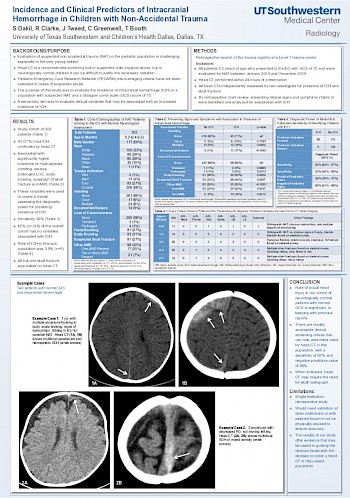
ABSTRACT INCIDENCE AND CLINICAL PREDICTORS OF INTRACRANIAL HEMORRHAGE IN CHILDREN WITH NON-ACCIDENTAL TRAUMA
PURPOSE Although head CT is a recommended screening tool in suspected child physical abuse, it is sometimes difficult to justify the radiation in neurologically normal children. The Pediatric Emergency Care Research Network (PECARN) criteria for neuro-imaging have been validated in all ages, but not in cases of suspected abuse. The purpose of this study was to evaluate the incidence of intracranial hemorrhage (ICH) in a population with suspected non-accidental trauma and a Glasgow coma scale score of 15. A secondary aim was to evaluate clinical variables that may demonstrate an increased incidence of ICH.
METHODS/MATERIALS The study cohort, identified by search of the trauma registry of a tertiary trauma center, consisted of patients under 2 years of age who presented to the ED and were evaluated for non-accidental trauma with a GCS of 15 between January 2010 and December 2016. All subjects had a head CT within 24 hours of presentation. All CTs were independently reviewed by two radiologists, assessing for presence of ICH and skull fractures. Patient charts were reviewed to identify presenting signs and symptoms, and variables were analyzed. Abbreviated injury scores (AIS) for all body regions as well as injury severity scores (ISS) were extracted from the trauma registry.
RESULTS The study cohort consisted of 302 patients. Sixty-three (21%) of the cohort had confirmed ICH. There was a significantly higher incidence of multi-episode vomiting, seizure, prolonged LOC, scalp bruising, suspicion of skull fracture, and altered mental status in the ICH group. Based on these clinical variables found to have a significant association with ICH, a model was built to maximize the sensitivity of predicting patients with ICH. The sensitivity of this model was 92%. Patients who presented with no variables that have an association with ICH accounted for 42% (n=129) of the population. The rate of ICH in this sub-population was 3.9%, and these patients had a significantly higher ISS score than the non-ICH patients in the subgroup.
CONCLUSION In keeping with previous reports, a significant portion of patients in our cohort had occult head injury. Our study assessed the usefulness of certain readily accessible clinical screening criteria for determining need for head CT in this population. With a positive predictive value of only 34% there will still be some patients with normal head CTs, however with a negative predictive value of 96%, these criteria are useful for excluding those patients who do not need a head CT.