Headline News
MR IMAGING OF SPINAL DROP METASTASES
MR IMAGING OF SPINAL DROP METASTASES
Steve Kralik MD
May 27, 2020
Accurate determination of the presence or absence of drop metastases is important for determining the prognosis and management of children with brain tumors. Features of high-quality MR imaging of drop metastases include high concordance between radiologists, definitive diagnoses (yes/no rather than indeterminate), thin section imaging capable of imaging small drop metastases, and reduction of CSF flow artifacts, which can obscure drop metastases that occur on the surface of the spinal cord. At a minimum, the ACR-ASNR-SPR and RAPNO recommendations for spine imaging include sagittal and axial T1W post-contrast imaging with 3 mm slice thickness in the sagittal plane and 4 mm thickness in the axial plane.1,2 Imaging can be improved using newer techniques including 3D T1W+C, 3D T2W, and DWI.2,3
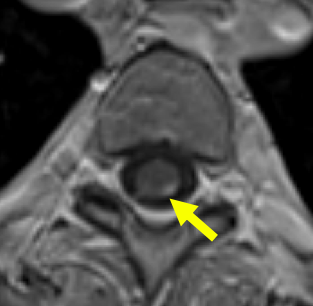

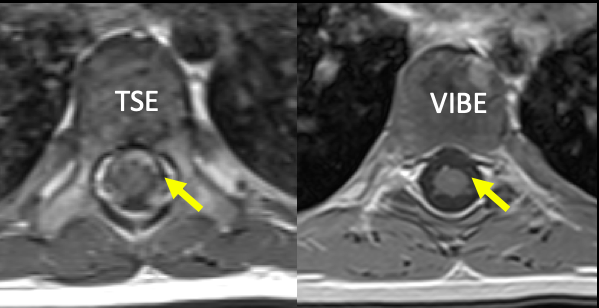
Post-contrast imaging using axial 3D T1W imaging techniques such as VIBE/FAME/THRIVE/LAVA should be considered in place of axial 2D T1W TSE/FSE as this sequence can eliminate CSF flow artifacts and thinner slices can be acquired with a shorter scan time.2,3 Sagittal 3D T2W imaging techniques such as CISS/FIESTA/SPACE/CUBE/VISTA allow for imaging with 1 mm slice thickness and multiplanar reformats, which is helpful for detecting small metastases and non-enhancing metastases.3,4 Use of a 2D T2W sequence is generally not adequate for identifying small drop metastases and 3D T2W sequences are far superior at achieving thin section imaging and high CSF-cord surface contrast. Higher myelographic quality but greater susceptibility effects may occur between CISS/FIESTA and SPACE/CUBE/VISTA sequences such that a trial phase may be needed to determine the optimal 3D T2W sequence from the MRI scanner.2 Lastly, DWI of the spine can be reliably performed with newer techniques such as RESOLVE or ZOOM and is particularly useful when the primary tumor is a high grade non-enhancing tumor.4
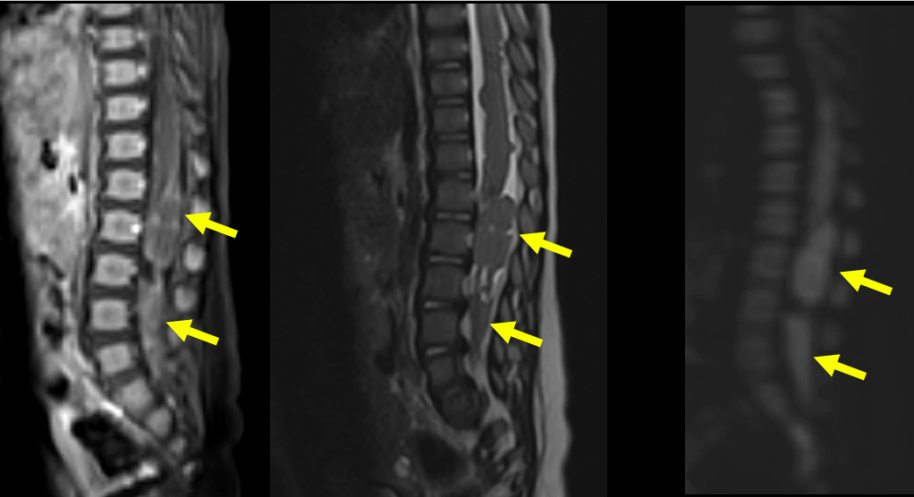
The optimal spinal drop metastases MRI protocol should achieve features of high-quality imaging listed above, but other factors may result in different MR imaging approaches between institutions. For example, one institution could establish a minimum protocol of sagittal 2D T1W and axial 3D T1W post-contrast sequences and in real-time decide to add 3D T2W and/or DWI imaging based on the appearance of the primary brain tumor. Other institutions may routinely include 3D T2W imaging to maintain a homogeneous protocol and avoid decision making in real-time. Ultimately, implementation of these newer techniques should result in overall improved clinical care for these patients through more accurate detection of disease.
Steve Kralik MD
Texas Children’s Hospital
Houston, TX
May 27, 2020
References:
- ACR-ASNR-SPR Practice parameter for the performance of Resonance Imaging of the pediatric spine. acr.org. 2019
- Warren K,E Vezina G, Poussaint TY, et al. Response assessment in medulloblastoma and leptomeningeal seeding tumors: recommendation from the Response Assessment in Pediatric Neuro-oncology committee. Neuro-Oncology 2018 20(1):13-23
- Kralik SF, O’Neill DP, Kamer AP, et al. Radiological diagnosis of drop metastases from pediatric brain tumors using combination of 2D and 3D MRI sequences. Clin Radiol. 2017 Oct;72(10):902.e13-902.
- Buch K, Caruso P, Ebb D, et al. Balanced Steady-State Free Precession Sequence (CISS/FIESTA/3D Driven Equilibrium Radiofrequency Reset Pulse) Increases the Diagnostic Yield for Spinal Drop Metastases in Children with Brain Tumors. AJNR Am J Neuroradiol. 2018 Jul;39(7):1355-1361
- Hayes LL, Jones RA, Palasis S, et al. Drop metastases to the pediatric spine revealed with diffusion-weighted MR imaging. Pediatr Radiol 2012 Aug;42(8):1009-13